Sonenshein Lab Works to Improve Breast Cancer Treatment
This story was written by Laura Castañón and originally appeared in Tufts Now.
Thirty years ago, Gail Sonenshein was studying cancer in immune cells when she read an article in the New York Times that would shape the rest of her career. The article described a new residency program in women’s health, part of an effort to improve treatment and outcomes for women at a time when most medical knowledge came from exclusively studying men.
“I woke up the next day and thought, well, I don’t see patients but I care about women’s health and I can do something about that,” said Sonenshein, who is now a professor of developmental, molecular, and chemical biology at Tufts University School of Medicine. “I decided to convert my whole lab over to breast cancer research.”
Since then, Sonenshein has directed all her efforts toward a better understanding of breast cancer and women’s health as a whole. She co-launched a women’s health research program at Boston Medical Center and served as its first director. She is developing tests to find evidence of carcinogen exposure in blood samples, and is working on a promising diagnostic and treatment for the most aggressive forms of breast cancer based around a protein called ADAM8.
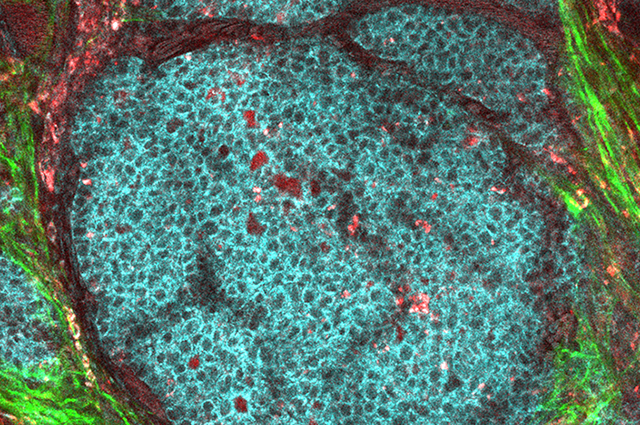
Sonenshein, who is also a professor at the Graduate School of Biomedical Sciences, and her colleagues discovered that the protein ADAM8 is on the surface of breast cancer cells and facilitates both the growth and spread of these cancers in mice. They recently developed antibodies that recognize and bind exclusively to ADAM8. Using an assay based on these antibodies, they showed that one third of all breast cancers express ADAM8 and that high levels of ADAM8 are associated with worse patient outcomes.
The work, published recently in Cancer Cell International, could help identify which cancers require more aggressive treatments. Sonenshein and her colleagues are also using these antibodies to develop treatments that would inhibit ADAM8, slowing or stopping the growth and spread of cancers with the worst prognoses.
“The most aggressive solid tumors are high in ADAM8,” Sonenshein said. “So if we can get this into the clinic and if it works as we hope, it’s going to be a big deal.”
Antibodies for ADAM8
When Sonenshein’s lab first identified ADAM8 as a potential target, they found that it affects cancers through two different mechanisms. One section of ADAM8, the metalloproteinase domain, helps new blood vessels form, which brings oxygen and nutrients to the cancer to help it grow larger. Another section, the disintegrin domain, modifies the outside of cancerous cells in a way that allows them to enter blood vessels and travel to other parts of the body.
This second part, the ability of a cancer to spread, is typically the most dangerous. Tumors that grow but don’t spread are usually easier to treat or remove. But Sonenshein found that most treatments in development against ADAM8 were only targeting the metalloproteinase domain—the piece that helps a cancer grow.
“If you target the growth, the cancer will be small but it can still spread, and it’s the spread that can kill you,” Sonenshein said.
Moreover, these treatments were not specific enough. They used small molecule inhibitors, which go inside a protein’s structure, and ended up impacting many proteins with metalloproteinase parts, not just ADAM8. Sonenshein and her team decided to take a different approach using antibodies.
As a proof of concept, the team started with a commercially available antibody that binds well to ADAM8 in mice and determined that tumors grew more slowly and didn’t spread as well when the researchers used the antibody to inhibit ADAM8. But the commercially available antibodies still had a five to ten percent chance of interacting with other proteins in the same family, so the researchers made plans to develop their own.
“We tried talking to different pharma companies to get them to work with us, but they weren’t interested because developing an antibody is much harder than a small molecule inhibitor and more expensive,” Sonenshein said. “I understand the preference for a small molecule inhibitor, but since it hadn’t worked for 20 years, maybe it’s time for a different strategy. Pharma wanted us to develop the antibody and then they would be interested in working with us.”
Despite the lack of support from pharmaceutical companies, Sonenshein intended to see the work translated into clinical use. She began developing ADAM8 antibodies in her lab at Tufts with research associate Nora Mineva. In 2014, the two women co-founded a company called Adecto Pharmaceuticals to develop both the antibody-based therapeutic and diagnostic for ADAM8-positive breast cancers.
With the assistance of grants from the National Institutes of Health and private foundations, the researchers have been able to design an antibody that exclusively binds to and stops ADAM8. They are now working to refine it before moving to clinical trials. If ultimately approved by the U.S. Food and Drug Administration, the therapy will provide a new targeted treatment option for breast cancers—including triple-negative breast cancers, which are particularly aggressive and don’t currently have effective targeted therapy options.
“Gail has taken this from identifying a target through the whole research process, and is now pushing it through development,” Mineva said. “That’s pretty unusual.”
Beyond Breast Cancer
Doctors will be able to use the diagnostic to determine if a tumor is high in ADAM8 and, if it is, use the therapeutic to impede the tumor’s growth and spread. And the possibilities go beyond breast cancer, Sonenshein said. The treatment could be effective for other cancers as well. Scientists have looked for ADAM8 in a variety of solid tumors and in every one of them, high ADAM8 levels have been associated with either the largest, fastest spreading, or deadliest tumors.
Late-stage gastric cancers, liver cancers, breast cancers—are all driven by the ADAM8 gene,” Sonenshein said. “If we come up with a treatment for one, given the results with other cancer driver genes such as HER2, it should work for the others.”
This potential impact for so many cancer patients is what keeps Sonenshein pushing forward with the research and the company when many of her friends and colleagues have retired. She is determined to see this work translated into treatments that will make a difference in people’s lives.
“If I have to work a couple of extra years until we obtain a partnership to get this into the clinic, it’s going to be worth it. I believe anti-ADAM8 targeted therapy is going to make a huge impact,” Sonenshein said. “That’s what keeps me going.”